How to Get Orthotics Covered by Medicare for Seniors
To get orthotics, and custom orthotics, covered by medicare for seniors you need to meet the eligibility criteria and have the orthotics deemed a medical necessity.
Key article takeaways
- The process to receive Medicare coverage for orthotic devices requires fulfilling specific eligibility standards and documentation requirements.
- Medicare provides coverage for orthotics, which fall under Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) when healthcare providers prescribe them for medical necessity.
- Be sure to fully understand Medicare Part A,B, and C before you process your claim as each bucket has different requirements.
- It's important to note the many pitfalls such as denial of claims and out-of-pocket expenses that can derail someone trying to get orthotics covered by medicare.
Eligibility Criteria and Medical Necessity
Medical Necessity Requirements
-
A Medicare-enrolled physician needs to write the prescription for the orthotic device after confirming its necessity for treating a particular medical condition.
-
The medical records need to contain detailed information about the diagnosis and functional limitations and how the orthotic device will help preserve or enhance the patient's condition.
Specific Conditions for Coverage
-
Beneficiaries with diabetes who have severe diabetic foot disease such as ulcers or deformities qualify for coverage of therapeutic shoes and inserts under Medicare. The program provides coverage for these items.
-
The coverage of orthotic devices for rehabilitation purposes after surgery depends on medical necessity and proper prescription from a physician.
-
Orthotic devices receive coverage for patients who have conditions like stroke, multiple sclerosis, or cerebral palsy because these conditions lead to mobility impairments.
Supplier and Provider Requirements
-
Orthotic devices must be purchased from suppliers who have enrolled in Medicare and fulfill its particular quality standards.
-
Suppliers need to accept Medicare assignment, which prevents them from charging more than the approved Medicare amount, thus protecting beneficiaries from increased costs.
The eligibility for coverage depends on both the prescribing physician and supplier meeting Medicare’s enrollment and assignment requirements.
-
Arthritis: The use of braces and orthotic inserts by patients with osteoarthritis or rheumatoid arthritis helps decrease joint stress which leads to better mobility and reduced discomfort. The PLOS ONE review showed that orthotic treatments effectively treat symptoms associated with arthritis.
-
Post-stroke Mobility Issues: The lower limbs receive stabilization through AFOs and KAFOs which improve gait patterns and reduce the risk of falls among stroke survivors. Research shows that these devices lead to superior functional results during post-stroke rehabilitation.
Clinical Evidence
Several studies have found that orthotic devices effectively enhance mobility while decreasing pain in seniors. The Journal of Foot and Ankle Research showed that personalized insoles effectively reduced plantar pressure in diabetic patients, thus lowering their risk of developing ulcers.
Medicare Coverage for Orthotics: An Overview
The process of obtaining Medicare coverage for orthotic devices requires knowledge of Medicare's different parts because seniors need this information to access necessary medical devices.
Medicare Part B: Outpatient Orthotic Coverage
Medicare Part B provides coverage for Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) when a Medicare-enrolled physician prescribes them for medical necessity. The coverage under Part B includes Ankle-Foot Orthoses (AFOs) and Knee-Ankle-Foot Orthoses (KAFOs) which serve to stabilize weak or deformed body parts and control motion in diseased or injured areas.
The Part B program of Medicare offers therapeutic shoes and inserts specifically for diabetic patients who have severe diabetic foot disease. The coverage includes both custom-molded shoes and inserts or extra-depth shoes with additional inserts specified per calendar year.
The beneficiary must pay 20% of the Medicare-approved amount after reaching the Part B deductible. The Medicare claims will not be paid by the program unless both the prescribing doctor and supplier are enrolled in Medicare.
Medicare Part A: Inpatient Orthotic Coverage
Medicare Part A provides payment for orthotic devices that patients require during their hospital or skilled nursing facility (SNF) stay for treatment purposes. The facility receives payment through bundled rates, which exclude separate billing for these devices.
The coverage for orthotic devices under Medicare Part B requires a Medicare-enrolled physician to write the prescription while the device must come from a Medicare-enrolled supplier.
Medicare Advantage (Part C): Plan-Specific Coverage
Private insurers who get Medicare approval offer Medicare Advantage Plans, which must provide benefits equal to Original Medicare Parts A and B. The coverage details including orthotic devices vary between different plans. The coverage benefits and cost-sharing requirements differ between plans. The Evidence of Coverage (EOC) document from the plan provider or direct contact with the plan provider will provide the necessary information to beneficiaries.
Medigap Policies: Supplemental Coverage
Medigap policies known as Medicare Supplement Insurance provide financial assistance for Original Medicare costs that exceed its coverage such as copayments, coinsurance and deductibles. Medigap policies do not extend orthotic device coverage beyond Original Medicare benefits but they help lower the expenses of purchasing these devices.
Steps to Obtain Medicare-Covered Orthotics
The process of obtaining Medicare coverage for orthotic devices requires a precise understanding of required procedures, together with compliance with specific guidelines. The following steps outline the process to obtain Medicare-covered orthotics:
Step 1: Medical Evaluation
-
Consultation: Make an appointment with a Medicare-enrolled physician who will evaluate the need for an orthotic device. Your physician will analyze your medical condition to establish whether an orthotic device serves a medical purpose.
-
Diagnosis: A proper diagnosis must be obtained to establish the medical requirement for an orthotic device. Orthotics serve patients who have diabetic foot complications and those who need them after surgery and those with neuromuscular disorders.
Step 2: Prescription and Documentation
-
Detailed Prescription: The physician must write a detailed prescription which outlines the specific orthotic device requirements along with its application purpose and medical treatment needs.
-
Supporting documents: The documentation process requires medical professionals to collect thorough medical records which include test results and clinical notes that validate the requirement for an orthotic device. The submission of correct documentation stands as a fundamental requirement for Medicare approval.
Step 3: Choosing a Supplier
-
Medicare-Enrolled Supplier: Choose a supplier who has enrolled in Medicare and follows all Medicare standards.
-
Verification: Verify the supplier's enrollment status through Medicare's supplier directory to confirm their authorization for DMEPOS item distribution.
Step 4: Submission and Approval
-
Claim Submission: The supplier will handle Medicare claim submission on your behalf by providing all required documentation and the physician's prescription.
-
Approval Process: Await Medicare's decision on the claim. The approval process may involve extra documentation or clarification. The timely response to requests is crucial because it prevents delays in the process.
The detailed process, combined with accurate documentation, enables seniors to obtain Medicare-covered orthotic devices successfully.
Common Challenges and How to Address Them
Medicare provides orthotic device coverage through certain conditions yet its beneficiaries may face various obstacles during the process. The knowledge of potential barriers together with their solutions helps create a more efficient process.
Denial of Claims
The main causes for claim denials stem from insufficient documentation and devices obtained from non-enrolled suppliers and medical necessity assessments. The solutions to these problems include proper completion of all paperwork and selection of Medicare-enrolled suppliers and detailed medical evidence for orthotic device approval.
Out-of-Pocket Costs
Medicare beneficiaries need to pay deductibles and coinsurance even though their medical expenses are covered by the program. People need to understand the possible costs they might need to pay.
Beneficiaries should investigate state-specific assistance programs, together with Medicaid, to obtain help with their additional costs. A Medicare advisor will help identify the resources that are available.
Navigating Plan Variations
The coverage of orthotic devices differs between Medicare Advantage Plans. People need to review plan details or seek advice from a Medicare advisor to understand their specific coverage and requirements.
Seniors who take proactive steps to handle typical problems and seek professional guidance will improve their chances of getting Medicare-covered orthotic devices.
Understanding Orthotics and Their Role in Senior Health
-
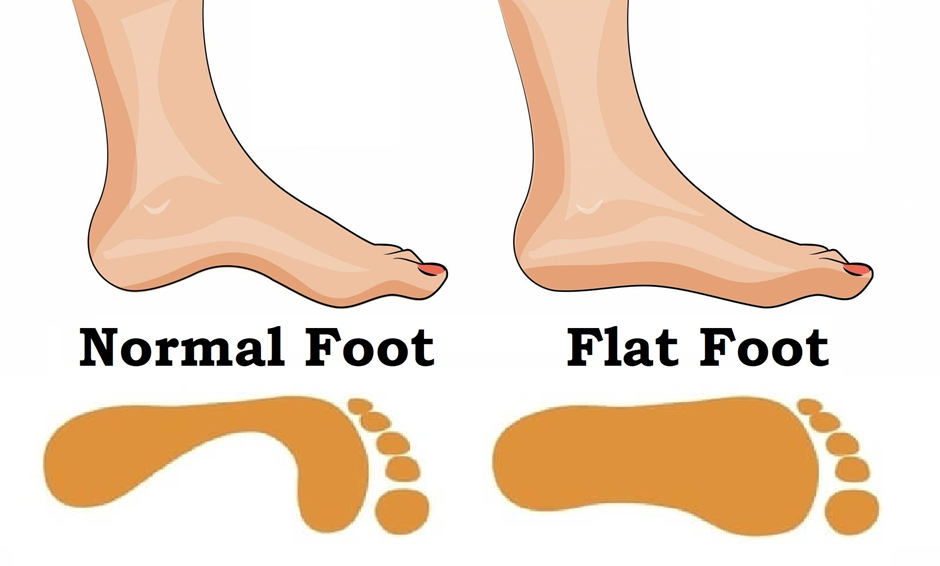
Foot Orthotics function as custom or prefabricated shoe inserts which provide support and alignment functions for foot improvement. Foot orthotics serve as medical devices to treat plantar fasciitis, flat feet and metatarsalgia.
-
Ankle-Foot Orthoses (AFOs) function as external braces that cover both ankle and foot areas to control ankle movement and position while providing compensation for weakness and correcting deformities. Medical professionals use AFOs to treat patients who have foot drop or stroke-related conditions.
-
Knee-Ankle-Foot Orthoses (KAFOs) reach from the thigh down to the foot to provide knee, ankle and foot support. KAFOs serve patients who experience severe lower limb weakness or paralysis including post-polio syndrome and severe arthritis.
Final Thoughts
Orthotic devices serve as essential tools in senior healthcare because they improve mobility while reducing pain and stopping medical complications from various conditions. The coverage process for certain orthotic devices through Medicare depends on medical necessity but patients must understand both eligibility requirements and documentation standards and supplier qualifications.
Healthcare providers should work with seniors and their caregivers to get required prescriptions and documentation. The selection of Medicare-enrolled suppliers who accept assignment will simplify the process and reduce out-of-pocket expenses.
The quality of life depends heavily on being knowledgeable and ready to access orthotic devices. Seniors who use available resources and understand Medicare coverage policies will obtain necessary support for maintaining their independence and well-being.