Plantar Fasciitis: The Ultimate Guide to Understanding, Preventing, and Treating Heel Pain
Plantar fasciitis is a foot condition resulting from the degeneration or inflammation of the plantar fascia. Microtears occur with the overuse of the plantar fascia, especially around the point where it attaches to the heel bone. These microtears lead to inflammation, which then results in sharp, stabbing heel pain. In some cases, the pain may also spread to the arch area.
This heel pain is most prominently felt with the first steps in the morning or after extended periods of rest. It can, however, begin to lessen after a period of activity.
Key Takeaways
-
Plantar fasciitis is the most common cause of heel pain. It results from inflammation or microtears in the plantar fascia.
-
Plantar fasciitis affects up to 10% of people, especially individuals who engage in high-impact activities like running, basketball, or people who spend extended periods on their feet.
-
The most common symptoms include sharp, stabbing heel pain usually felt with the first steps in the morning. This pain will often subside after walking for about an hour but may then return when you are resting again.
-
Plantar fasciitis is preventable with the right lifestyle adjustments, which include proper weight management, the use of supportive footwear, the use of orthotic insoles, rest, engaging in simple foot and calf muscle stretches, and properly conditioning your muscles before engaging in high-impact activities.
-
Surgical intervention is only necessary if other options have failed. This option is rarely needed, and when it is, it must be handled by a qualified orthopedic or podiatric surgeon.
-
Plantar Fasciitis can be better treated when diagnosed early. Without proper attention, the condition will worsen and may lead to chronic pain.
What is the Plantar Fascia?
The plantar fascia is a collagen-rich tissue that stretches lengthwise on the bottom of the foot, connecting the calcaneus (the heel bone) to the metatarsal heads (the base of the toes).

Some of its core functions include the following:
-
Arch Support – The plantar fascia is like the bowstring attached to the two ends of a bow, pulling it taut. With both ends of the plantar fascia attached to the heels and toes, respectively, the tension it creates between these points helps keep the arch shape, preventing it from collapsing.
-
Absorbing Impact Shock – As you walk or run, the foot hits the ground, sending shock waves up the leg. The arch, supported by the plantar fascia, absorbs the shock, spreading it evenly across the foot. This ensures that no single part of the foot takes on excess strain.
-
Gait Cycle Assistance and Movement Efficiency – The plantar fascia contracts and relaxes at different phases of the gait cycle. In the mid-stance phase, it stretches, storing elastic energy. This supports the arch as it absorbs the impact shock. In the push-off phase, it contracts, raising the arch, an action that converts the stored elastic energy into forward propulsion. This gives the arch its spring-like action, known as Windlass Mechanism. Without this mechanism, movement will be inefficient.
-
Maintaining Foot Shape – The plantar fascia helps keep the bones of the foot in shape while in motion or at rest. It also helps them perform their supportive functions efficiently.
Because the plantar fascia is constantly exposed to these actions described above, it can easily experience microtears, inflammation, and degeneration, resulting in plantar fasciitis
What Causes Plantar Fasciitis?

Let’s start by looking at the primary causes, followed by contributing risk factors.
Primary Causes of Plantar Fasciitis
Plantar fasciitis is generally caused by overuse or repetitive stress on the plantar fascia. There are, however, different factors that can be the underlying causes or triggers. Let's look at the most common of these.
-
Repetitive Activities Leading to Overuse – This is the leading cause of plantar fasciitis. Activities like long-distance running, sports that require a lot of running and jumping (basketball, volleyball etc.), and a sudden increase in activity or intensity without previous conditioning, all fall into this category. When the plantar fascia is not given enough time to recover, more microtears will occur, and the condition will worsen.
-
Improper Footwear – Footwear without proper arch support, shock absorption, and cushioning can increase the stress on the plantar fascia. Examples include shoes with worn-out soles, flat soles, or high heels because they can alter the foot's mechanics, putting more pressure on the plantar fascia and increasing the risk of plantar fasciitis.
-
Pre-existing Foot Conditions – Any pre-existing foot conditions that affect the foot's mechanics can easily lead to plantar fasciitis. Some examples of such pre-existing conditions include flat feet, overpronation, high arch, or leg length discrepancy. These conditions all affect the way the body's weight is distributed, significantly increasing the stress on parts of the plantar fascia.
-
Tight Calf Muscles or Achilles Tendon – Tight calf muscles or Achilles tendon reduce flexibility, restricting ankle dorsiflexion (your ability to point your foot upward). This lack of flexibility will put more stress on the plantar fascia by making it overstretch during movement.
Secondary (Contributing) Risk Factors
Other factors that can increase the risk of plantar fasciitis include the following:
-
Obesity – With excess body weight, the plantar fascia has to deal with more weight than it should. This leads to an increase in the mechanical stress that it has to deal with. Generally, a BMI of 30 and above increases the risk of plantar fasciitis.
-
Lifestyle and Occupational Requirements – Jobs or lifestyles where you are on your feet most of the day increase your risk factor. Nurses, waiters, factory workers, teachers, and cops are some common examples.
-
Degeneration from Aging – The natural process of aging affects the plantar fascia, leading to a weakening or degeneration of the tissue. As the plantar fascia weakens, it gets more susceptible to injuries, which can lead to plantar fasciitis.
-
Health Conditions – Health conditions like diabetes, arthritis, and joint hypermobility can increase the chances of plantar fasciitis occurring. Diabetes can cause nerve and circulation issues, joint hypermobility causes foot alignment issues, and arthritis, especially rheumatoid arthritis or ankylosing spondylitis, can cause inflammation or trigger joint stiffness.
Symptoms of Plantar Fasciitis
Some of the common symptoms that can be indicative of plantar fasciitis include:
-
Sharp Heel Pain in the Morning – The reason pain is concentrated to first thing in the morning is that during the period of rest, the plantar fascia tightens quite a bit. So, when you try to walk after resting, it is suddenly stretched, resulting in the sharp, stabbing pain you feel. This pain will usually ease off after a few minutes as the tissue gets more flexible.
-
Heel Pain that Gets Worse with Time – At first, the heel pain may be mild. However, if it is left untreated, it will gradually worsen and may then become chronic, making it more difficult to treat.
-
Pain Type – Heel pain from plantar fasciitis is often described as stabbing, sharp, and even burning.
-
Pain that Gets Worse After Activity – Unlike some other types of pain that worsen with increased activity, this type will usually worsen after the activity. This is because the tissue becomes flexible during the activity but begins to stiffen after the activity, resulting in a delayed pain response.
-
Tightness and Stiffness in the Foot – You may feel stiffness or tightness in the bottom of the foot, especially around the arch. It can also feel like something is pulling on the tissue, or you are experiencing some cramping when you walk barefoot or do some stretching.
-
Mild Swelling and Warmth – If the condition has become acute, there may be some swelling around the heel area. It may also feel warm to touch. This swelling is often mild, so if the swelling is severe, it may be pointing to a different condition.
Given all of the above, to know if you have plantar fasciitis, ask yourself the following questions:
-
Do I feel a sharp, stabbing heel pain with my first steps of the day?
-
Do I feel the pain easing off after I have walked around for a few minutes?
-
Does this pain return or worsen after I have spent a long time on my feet or sitting?
-
Do I find it difficult to walk barefoot on hard floors and surfaces?
-
Does the pain get worse after an intense activity and not during the activity?
Answering yes to 3 or more of the above is a strong indication that you may have plantar fasciitis. However, since some other conditions, like heel spurs, fat pad atrophy, and Achilles tendinopathy, can have similar symptoms, you may need to visit your podiatrist for confirmation.
You can also do this simple self-test to confirm that the pain is related to the plantar fascia. While seated, try to pull your toes upward. This will stretch the plantar fascia. If you feel pain when you pull your toes, then there’s an issue with the plantar fascia.
Diagnosing Plantar Fasciitis
When you visit your podiatrist to confirm if you have plantar fasciitis, you can expect to provide the following:
-
Medical History Questionnaire – You will be asked certain questions to ascertain your medical history. This will include any history of foot conditions, injuries, aches or pains, changes in activity level, occupation, as well as the type, location, and timing of the pain.
-
Physical Examination - Your doctor will physically examine your feet. This will involve pressing the heel to check for pain, checking for tight calf muscles, gait, swelling, bruising, redness, and other related factors.
-
Scans - Scans may also be required to rule out other possible causes or check for the true state of the plantar fascia.
The examination will confirm whether or not it is plantar fasciitis.
How to Prevent Plantar Fasciitis

The following tips can help prevent plantar fasciitis:
Wear the Right Footwear
This is the first thing to look at. The right footwear should have the following features:
-
Arch Support – This ensures that the plantar fascia is not overworked trying to keep the arch up.
-
Shock Absorption – The shoe’s ability to absorb some of the impact shock reduces the amount of shock transferred to the arch, further easing the workload on the plantar fascia.
-
Firm Heel Counter – This is important to help keep the heel in place. Once heel stability is achieved, proper alignment and balance is easier to achieve, reducing the strain on other parts of the foot.
-
Slight Heel Elevation – The ideal shoe should not be flat or high-heeled. They should offer a slight heel elevation to reduce strain on the calf muscles and the Achilles tendon.
-
Right Fit – Ensure that your shoes fit properly. They should have enough toe box space, and wiggle room for both circulation and comfort.
Perform Regular Calf and Feet Stretches
Regular calf and foot stretches can help reduce stiffness in the calf muscles and Achilles tendon. Doing these stretches 2 to 3 times every day will increase both their flexibility and strength.
Some examples of simple stretches include:
-
Using your hand to pull the toes towards you while you are seated.

-
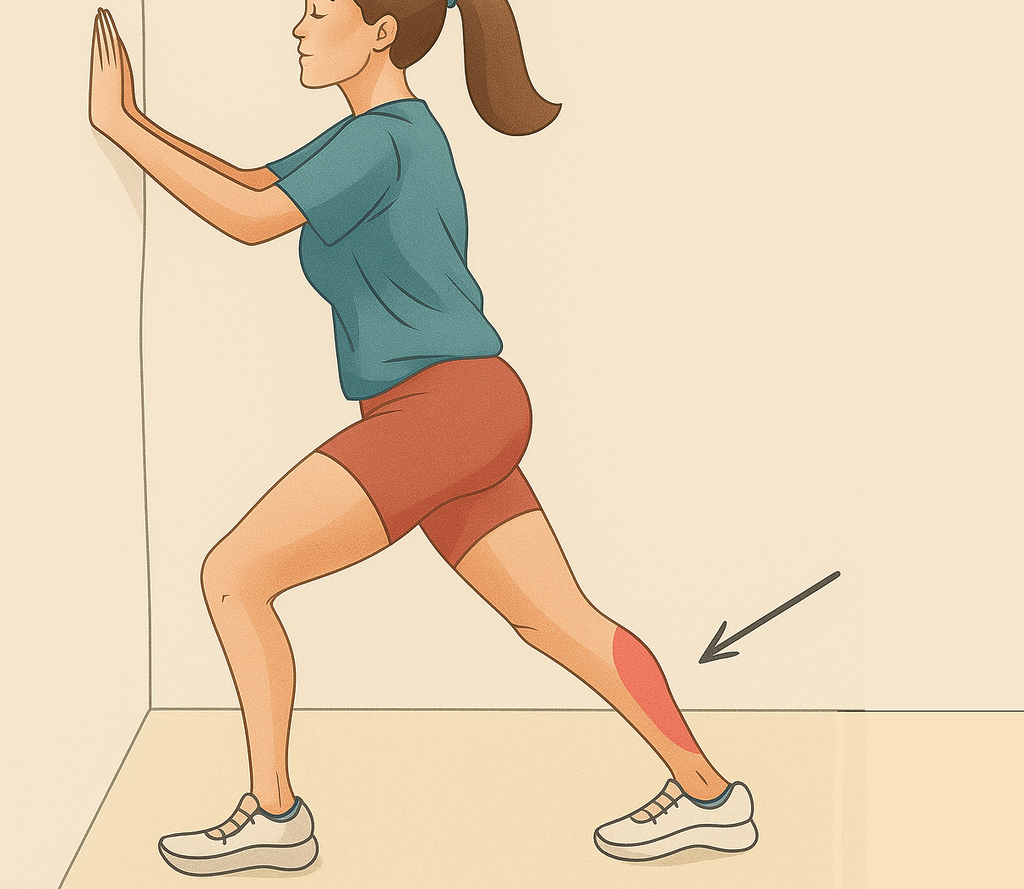
Calf stretch - With both arms on the wall and the feet slightly apart, move one leg back and place the heel of that foot on the floor. This will stretch the calf muscles. Repeat with the second leg.

-
Rolling your foot over a tennis ball.

According to Dr. Emily Chen, a physical therapist, the key is consistency. According to her, "daily stretching not only prevents plantar fasciitis but also improves overall foot resilience, reducing injury risk."
Muscle Strengthening Exercises
Engage in exercises that strengthen the muscles of the foot to ensure that the arch has the right support structure. When the right support is in place, the plantar fascia will not be overworked.
Some simple muscle-strengthening exercises include:
-
Balancing Exercises - Stand on one foot and try to maintain balance. You can do that for both feet.

-
Towel Scrunches - Using your toes to grip a towel and pulling it toward you.
-
Marble Pickup - Attempting to pick up small items like marbles with your toes.

Use Orthotic Insoles
Orthotic insoles can be a great help in preventing the occurrence of plantar fasciitis. This is because the right insole will:
-
Provide adequate arch support
-
Provide shock absorption
-
Make the foot comfortable
-
Help with weight distribution, foot alignment, and balance
To enjoy the full benefits that an orthotic insole can provide, you must get the right fit and right design. A good option is the Custom Orthotics for Plantar Fasciitis offered by Stride Soles.
Exercise Responsibly
Exercises are important, but when done wrongly, they can be harmful. Never start a high-impact exercise without properly conditioning your body. Always start gradually and increase intensity slowly. This will give the muscles time to adjust and not get hurt by a sudden increase in exercise intensity.
Other Tips
Other important tips that can help prevent this condition include:
-
Maintaining a healthy weight. When the feet have to carry more weight than they ought to, all the structures, including the plantar fascia, are put under increased strain.
-
Do not walk barefoot on hard surfaces for extended periods because this can increase the strain on the plantar fascia.
-
Do exercises that improve posture and flexibility. This will help with balance, tight hamstrings, and alignment issues.
-
Have days when your feet can rest from exercising so the plantar fascia can recover.
-
If you spend a lot of time on your feet every day, take 1 to 2-hour breaks to rest the feet.
-
Always pay attention to your feet. If you begin to feel discomfort or pain, do not just dismiss it. Catching this condition early increases your chances of having it resolved quickly.
In concluding this section on prevention, Dr. Mark Rivera, a certified podiatrist put it this way, "prevention is about building habits that support your feet long-term. Investing in good shoes, stretching regularly, and listening to your body’s signals can keep plantar fasciitis at bay, even for high-risk individuals."
How to Manage Plantar Fasciitis

Managing plantar fasciitis entails taking steps to reduce the pain and discomfort so that you can go about your daily activities more comfortably. While this does not necessarily mean treating the condition, it is usually a first step in this direction, which is why it is often referred to as the conservative treatment option.
Let’s look at the options that fall under this category.
Rest and Modify Your Activities
When there is a flare-up and you are in serious pain and discomfort, the very first thing to do is give the foot a rest. It may sometimes be necessary to put the foot up and not put any weight on it for a while. If this is not possible, reduce the level of activity you engage in so that the plantar fascia can have time to recover. You can also switch to other low-impact options like cycling or swimming.
Exercises to Strengthen and Stretch the Muscles
This is the same process described for prevention. Doing the stretches described above can reduce the tension on the calf muscles, Achilles tendon, and the plantar fascia. These activities, when carried out with consistency, will increase the speed at which recovery occurs.
To reduce the pain that usually comes with the first steps in the morning, you can do a towel stretch before taking those first steps. Just before you get out of bed in the morning, wrap a towel around the ball of your foot and gently pull back, towards you, holding for about 30 seconds. This will gradually reduce the tension on the plantar fascia. Repeat this about 3 times before you take your first step. You should experience less pain.

Ice Therapy
To alleviate the inflammation and pain that is often associated with plantar fasciitis, you can place an ice pack on the bottom of the foot. You can also roll the arch of the foot over a bottle of frozen water. Do this for between 15 to 20 minutes about 3 times each day.
Supportive Footwear
Wearing the right footwear helps with both the prevention and management of the condition. So, remember to use footwear that offer:
-
Arch support
-
Shock absorption
-
Firm heel counter
-
Cushioning for comfort
-
Mild heel height
-
Wide toe box
Remember to avoid shoes with:
-
Flat soles
-
High heels
-
Worn support
-
Tight laces or a tight fit
Your choice of footwear can make an immense difference in how quickly you will be free of plantar fasciitis. You can also insert orthotic insoles for plantar fasciitis into your footwear to get the right support and comfort.
Medication
Pain and Inflammation can be managed with medication. NSAIDs, like ibuprofen or naproxen, can be used to help reduce the pain and inflammation. This is, however, a short-term measure which do not address the root cause. They can nonetheless be necessary when you are dealing with a lot of pain and discomfort. Read our Plantar Fasciitis Medication Guide.
Weight Management
Losing just a little weight (if overweight) can have a massive impact on the state of the plantar fascia. Excessive weight puts this tissue and other supporting structures under a lot of strain, increasing the occurrence of different foot conditions, including plantar fasciitis.
The more weight you can lose, the more strain you take off the plantar fascia. This is therefore something that you should give attention to both for prevention and treatment.
Physical Therapy
Physical therapy can be helpful in the management or conservative treatment of plantar fasciitis. Working with a certified physical therapist, a personalized plan can be developed to help address the issue. This can include:
-
Massages to reduce stiffness and increase flexibility
-
Posture and gait correction to improve balance and alignment
-
Laser or ultrasound therapy to improve the healing process while reducing pain and inflammation
-
Taping technique to improve support, reduce strain on the plantar fascia, and enhance alignment.
The best methods to be used will be determined by your physical therapist.
Night Splints
This can be used to gently flex the plantar fascia through the night as you sleep. Doing this will ensure that the pain associated with the first steps in the morning is reduced.
If after doing all of the above the condition still does not improve, then it may be time for more aggressive treatment methods.
How to Treat Plantar Fasciitis
The treatments we will be looking at now will become necessary if the previously discussed treatment methods (referred to as conservative treatment methods) do not yield the desired results after about 6 to 12 weeks.
To handle these more severe or chronic cases of plantar fasciitis, the following advanced treatment plans may be employed:
Corticosteroid Injections
This method, which is employed to quickly reduce inflammation and pain, involves injecting corticosteroids (strong anti-inflammatory medication) directly into the inflamed area, which is the arch or heel areas. This injection will quickly provide relief from pain, and allow you return to active duties faster.
These injections should, however, not be given repeatedly as they can weaken the plantar fascia and increase the risk of further damage to it. It should only be used for very short-term relief.
Platelet-Rich Plasma (PRP) Injections
This method uses your body's natural healing properties to promote the healing of the plantar fascia. To do this, your blood sample is taken, and a concentrate of your platelets is extracted from it. This is then injected into the plantar fascia.
While this method can accelerate the healing process naturally, it can also be expensive. It may also take weeks, even months, before you begin to see real results.
This method will be ideal for anyone who wants a completely drug-free treatment option.
Extracorporeal Shockwave Therapy (ESWT)
In this method, high-energy sound waves are used to promote tissue regeneration, helping the body naturally repair itself. This method, which is often used when others have not yielded the desired result, is non-invasive and only targets the affected area.
This may be an ideal option for chronic cases that have defied intervention for over 6 months. To get the desired result, treatment may need to go on for several sessions. Since the treatment process causes some discomfort, it's important to mentally prepare for it.
Percutaneous Tenotomy (Tenex Procedure)
In this procedure, damaged tissues are removed, allowing healthy tissues to heal faster. Carrying out this procedure involves a minimally invasive process where a small probe is inserted into plantar fascia through a microincision and guided by an ultrasound scanner. This probe breaks up the damaged tissue and sucks them out.
This is a minor surgery with a fast recovery time of a few weeks. With this procedure, chronic pain can be reduced without an extensive surgical procedure. It is best suited for cases where it is confirmed that the plantar fascia is thickening or degenerating.
There may be need for some physical therapy after the procedure to aid the recovery process.
Gastrocnemius Recession
This procedure is used when the underlying cause of plantar fasciitis is tight calf muscles. In this procedure, the gastrocnemius muscle is lengthened to ease the tension transferred to the plantar fascia and the Achilles tendon by the shortened muscle.
Once done, recovery can take up to 12 weeks and physical therapy will be required to help the muscles get back to full strength. It may take up to 6 months to see the full effects of the surgery.
Plantar Fascia Release Surgery
This treatment option is meant to offer permanent relief from pressure and tension on the plantar fascia. It should, however, be done only as a last resort, when other less radical treatments have failed.
This surgery, which can be open or endoscopic, involves surgically cutting a small part of the plantar fascia to ease the stress on it. The procedure is effective for dealing with the worst cases of plantar fasciitis because it can result in a significant reduction in pain when it is successful.
Recovery time for this surgery can be as long as 12 weeks. Of this period, 4 to 8 weeks will be with minimal load bearing. After this, physical therapy will be required to help you get back to full function.
This surgery should only be performed by qualified podiatric or orthopedic surgeons. This is important to reduce the risk of nerve damage, infections, or arch instability. According to Dr. Mark Rivera, who is an orthotic surgeon, "surgery is a last resort due to risks and variable outcomes. Exhaust conservative options first and choose a surgeon experienced in foot procedures."
Alternative Treatment Options
Aside from the orthodox treatment options discussed above, there are some unorthodox methods that can also be employed. These include:
-
Acupuncture – This treatment can help relax foot muscles and improve blood flow.
-
Dry Needling – This method is similar to acupuncture and involves dry needling targeted trigger points in the foot and calf muscles to release tension in them.
In many cases, the treatments discussed above are combined for a more effective outcome. Your podiatrist will be in a good position to determine which solutions will be best for your case.
Conclusion
We’ve taken some time to discuss plantar fasciitis, its causes, prevention, and treatment options. The goal of this article is to help you maintain proper foot health, whether you are already suffering from the condition or simply want to prevent it.
For those already dealing with the condition, we’ve discussed several tips to help you manage and even treat it effectively. Follow this advice given by Podiatrist Dr. Lisa Patel, "start with conservative treatments and give them time. Most patients avoid surgery by sticking to a disciplined routine of stretching, proper shoes, and rest."
Here’s to your feet’s health!
Plantar Fasciitis FAQ
What Causes Plantar Fasciitis?
Plantar fasciitis is often caused by overuse, repetitive stress, obesity, poor footwear, tight calf muscles, and spending so much time standing or walking on hard surfaces.
What are the Main Symptoms of Plantar Fasciitis?
Sharp, stabbing heel pain, especially with the first steps in the morning or after resting the foot for a while. The pain will often reduce as you keep walking but returns when you rest.
Can Plantar Fasciitis Heal on its Own?
Mild cases can get better if you give the feet rest, allowing it time to heal itself and implement the simple self-care procedures discussed in this article. If, however, it is left unattended to, it will get worse and may then require more severe intervention.
What are the Best Self-Care Methods for Plantar Fasciitis?
Rest, ice therapy, use of orthotics, supportive shoes, foot and calf stretches, and pain medication.
Can Plantar Fasciitis be Prevented?
Yes! With the right lifestyle choices like proper weight management, use of orthotic insoles, giving he feet enough rest to avoid overuse, using supportive footwear, and doing regular foot and calf stretches.
How Do I Know If I have Plantar Fasciitis?
If you have sharp heel pain with the first steps in the morning, which gets better after you’ve walked for a while, or you feel pain when you pull your toes up toward you while seated, or notice that the heel pain returns after you have engaged in activities for a while, then you may have plantar fasciitis. You will, however, need a podiatrist to confirm the diagnosis.
Can I Still Run with Plantar Fasciitis?
Running with plantar fasciitis can worsen the condition and make recovery more difficult. You should give it a rest or switch to less high-impact activities like swimming.
When Should I Visit a Doctor?
You should see your doctor or podiatrist if the pain has not reduced despite the home treatments. If it's getting worse, then see a doctor.
Does Surgery Offer a Lasting Solution?
When successful, surgery can provide a lasting solution to plantar fasciitis. It is, however, to be considered only as a last resort because it comes with a number of risks. You should only consider this option if other less risky treatment options have failed.